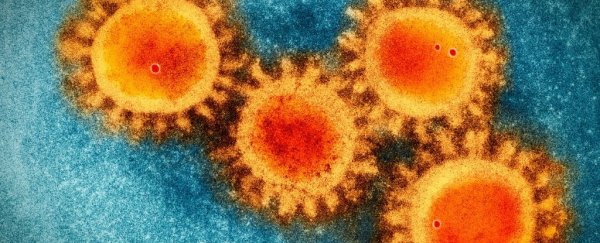
Coronavirus strains are viral variants considered to be functionally unique enough to stand out in a significant way.
Mutations can occur spontaneously in the virus's genome as its particles - or virions - copy themselves inside a host's cells. Most genetic changes have little impact on the virus's function, but can still be used by epidemiologists to trace patterns of spread through a community.
Some mutations might make the virus less efficient, reducing their ability to spread or triggering stronger immune responses in the host. These will usually die off as they struggle to compete with more silent, more efficient versions.
Every now and then a change will give a virus an even bigger advantage, helping it spread faster still by sticking to new receptors or by avoiding detection by the immune system.
Scientifically speaking, there is no standardised difference in physiology, chemistry, or genetic sequence that automatically defines a virus as a new strain.
Such 'changed' viruses that operate better or worse, or simply function differently, are often catagorised as strains to make them easier to study and predict their spread across a population.
How many SARS-CoV-2 strains are there?
There are a number of variants of SARS-CoV-2, but so far only a handful that are functionally different enough to be considered strains.
By mid-2020, as the pandemic was raging around the globe, virologists had distinguished six isolates of the virus that were structurally different enough to raise questions over whether they might be of serious concern. These were given simple titles with the letters L, S, V, G, GR, and GH, reflecting the genes responsible for differences in their surface proteins.
Based on the fact G strains were found to be slowly increasing while L and V seemed to be disappearing, virologists argued their individual characteristics might be distinct enough to affect how they functioned.
In September, infections were being reported among minks in North Jutland, Denmark, which possessed a unique set of mutations. Just a dozen people were reported to have this variant, referred to as Cluster 5, with the viruses showing signs of a reduced sensitivity to neutralising antibodies. The outbreak was contained following a major cull of minks in fur farms across the nation.
Another isolate identified in the UK that same month was found to have nearly two dozen mutations in places that prompted concerns over its ability to infect new hosts. By December it was becoming clear that this 'UK variant' of SARS-CoV-2 was representing a greater proportion of cases.
Complicating matters is the question of whether the variant was truly better at spreading, or simply taking advantage of breaking ground into a susceptible new population - something described as the founder effect.
A variant identified in South Africa in December was the first SARS-CoV-2 isolate to really grab the attention of epidemiologists. This 'variant of concern', or VOC 202012/01, spread quickly through areas that SARS-CoV-2 was already well established, making it unlikely its rapid movement was caused by the founder effect.
Is there a less confusing way to remember all of these strains?
By mid-2021, the World Health Organisation realised it needed a better way to communicate which variants we need to pay close attention to.
The ammended system applies Greek letters to share news of variants with the public. For example, the British variant B.1.1.7 can instead be referred to as the Alpha strain. B.1.351, first discovered in South Africa, can be called Beta. Gamma refers to the strain noted in Brazil, coded P.1, and the concerning lineage of a strain first identified in India, B.1.617, can be called Delta.
It doesn't change how researchers apply their coding, but for the rest of us it's a far simpler way to keep track.
Are any of the SARS-CoV-2 strains more deadly than the rest?
Data are too limited at the moment to state with confidence whether any of the strains are more likely to cause serious illness or death.
Some early studies suggest the Alpha variant might not only spread 50 to 70 percent faster, but could be as much as 40 percent more deadly, possibly as a result of its improved ability to infect.
More recent observations suggest the Delta variant could result in more hospitalisations than Alpha.
As vaccination programs roll out in many developed nations, there are also concerns that strains might develop a resistance to one or more of the vaccines.
Should we be concerned about future strains of SARS-CoV-2?
It's impossible to predict how a virus will mutate, let alone evolve new traits. Yet with so many people infected in populations all over the world we can be confident new strains will continue to emerge.
On the positive side, SARS-CoV-2 seems to mutate rather slowly, at least compared with pathogens such as HIV.
In terms of the long-game, this could also be considered a downside. A close look at the evolution of pandemics throughout history, such as the Spanish Flu, suggests new strains become less deadly with time as symptomatic hosts are isolated or die, and 'stealthy', low-impact strains become more dominant in carriers. Slower mutation rates could, in theory, cause a pandemic to drag out.
Eradicating the current strains of SARS-CoV-2 will take a monumental global effort. If history is anything to go by, there will be strains of this virus in our population for a long time to come.
All Explainers are determined by fact checkers to be correct and relevant at the time of publishing. Text and images may be altered, removed, or added to as an editorial decision to keep information current.