New research reveals that the process of remembering something long-term comes at a cost – specifically, inflammation in the brain and DNA damage in nerve cells, as the memories get 'fused' into neurons and stored.
The international team of researchers suggests that memory formation is not unlike making an omelet by breaking a few eggs: some careful destruction is required before a new memory pattern can form.
Based on tests on mice carried out for the study, this happens inside the hippocampus, a part of the brain already known to be the primary storage locker for our memories and crucial to the process of remembering.
"Inflammation of brain neurons is usually considered to be a bad thing, since it can lead to neurological problems such as Alzheimer's and Parkinson's disease," says neuroscientist Jelena Radulovic from the Albert Einstein College of Medicine in New York.
"But our findings suggest that inflammation in certain neurons in the brain's hippocampal region is essential for making long-lasting memories."
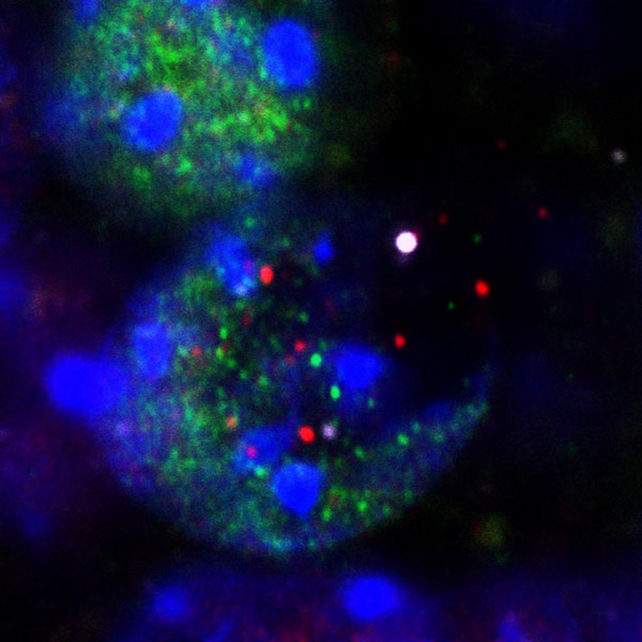
The team triggered episodic memory in mice with brief, mild electric shocks. Close analysis of hippocampal neurons revealed the activation of genes in the Toll-Like Receptor 9 (TLR9) pathway, important for inflammatory signaling. What's more, this pathway was only activated in clusters of neurons, which also showed DNA damage.
While breaks in DNA in the brain happen often, they're usually repaired very quickly. Here, the changes seemed more significant, with biological processes usually linked to cell division apparently being used to organize neurons into memory-forming clusters without dividing the cells.
The inflammatory editing mechanisms in the mice lasted a week, after which the memory-storing neurons were found to be more resistant to outside forces. This suggests that memories are then locked in for good and protected from external interference. Something similar likely happens in the human brain, too.
"This is noteworthy because we're constantly flooded by information, and the neurons that encode memories need to preserve the information they've already acquired and not be distracted by new inputs," says Radulovic.
When the same TLR9 inflammatory pathway was blocked in the mice, they could no longer be trained to remember the electric shocks. The absence of TLR9 also led to more severe DNA damage, not unlike that seen in neurodegenerative disorders.
Blocking the TLR9 pathway has been proposed to treat or prevent long-term COVID-19, but this study suggests that the idea may need rethinking. Most of all, though, it's an intriguing new insight into how memories are stored in the brain.
"Cell division and the immune response have been highly conserved in animal life over millions of years, enabling life to continue while providing protection from foreign pathogens," says Radulovic.
"It seems likely that over the course of evolution, hippocampal neurons have adopted this immune-based memory mechanism by combining the immune response's DNA-sensing TLR9 pathway with a DNA repair centrosome function to form memories without progressing to cell division."
The research has been published in Nature.
